10 News – Tampa Bay Sarasota
Sea lice are popping up all over Gulf Coast beaches. While many sightings are along the panhandle, biologists say they expect to start seeing more move south along the coastline.
Sea lice are microscopic and impossible to spot in the water. They aren’t the kind of lice you may be thinking of.
Sea lice are actually jellyfish larvae and while they are tiny, they still have the same stinging cells as a full grown jellyfish, and they’ll leave a mark.
The rash they cause is called sunbathers eruption. Often time the sea lice will get caught beneath a swimmer’s bathing suit. Because they sting like jellyfish, sunbathers eruption can be treated just like a jellyfish sting.
While they can be found throughout the year, sea lice are most active from the months of April through August.
To learn more about sea lice, please continue reading below:
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
SEA LICE or Seabathers Eruption
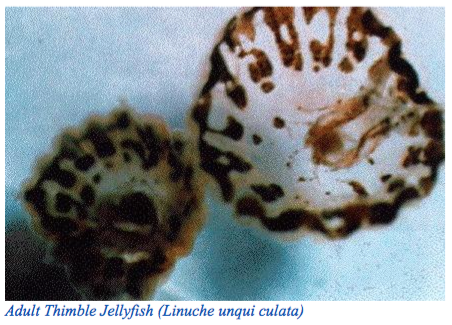
Adult Thimble Jellyfish (Linuche unqui culata)
CLINICAL ARTICLES SEABATHER’S ERUPTION OR “SEA LICE”: New findings and clinical implications
Mary T. RusselI, RN, MSN, CCRN, CEN, and Robert S. Tomchik, MD, MPH, Boca Raton, Miami, and Fort Lauderdale, Florida.
History
For the past 11 years, during the months of March through August, residents and tourists along 250 miles of Florida’s southern Atlantic coastline have complained of an annoying pruritic rash, primarily within areas covered by bathing suits. Although this problem has existed since the early 1900s at least, it has not been formally recognized and understood until recently. The first study (a retrospective case review of ED cases seen during 1992) and a sample population survey were conducted at Boca Raton Community Hospital. The outbreaks appear to have intensified in the last 4 years, as reflected in the number of cases reported as well as the severity of response in individual cases. Because most affected people treat themselves, it is difficult to determine the total annual number of cases. However, a conservative estimate of 10,000 cases in 1992 can be made. A sample population survey of 1433 persons who went swimming within the apparent geographic center of the outbreaks indicated that one of every four persons that went swimming had the dermatitis.
Because the Sunshine State has a significant tourist population, people who have the rash return to their respective states or countries, seeking follow-up care from their local health care facilities. This has prompted calls to Florida’s Public Health Offices and emergency departments, requesting information as to the origins of the rash and recommendations for treatment. Many persons expressed confusion and fear that they had contracted a communicable disease, such as venereal disease, chickenpox, or measles.
Periodic outbreaks have existed before this decade, and it is possible that this form of dermatitis has been around for centuries. Fishermen have long been acquainted with it, affirming reports in Cuba, Puerto Rico, Mexico, and the Caribbean islands. Names such as “sea poisoning,” “sea critters,” and “ocean itch” have been used as descriptions of this seasonal affliction. A Bahamian old wives’ tale specifically warns against ocean swimming between Mother’s Day and Father’s Day yearly.
A local resident from Miami, Florida, described bathing on the beach in the spring of 1903 as the “year we were all poisoned… with some kind of rash which set up an intense itching. It was not so bad for us as we could stay home and doctor ourselves with lotions but the poor men having to work in the fields or hot packing houses were the ones who really suffered.”
In 1949, Dr. Wiley Sams gave a detailed description of his 12 years of observations and research of “an acute form of dermatitis which occurs within a short time after bathing in the ocean.” He recorded the distribution and histology of the lesions, their clinical presentation, and his theory that seabather’s eruption was caused by “some living, microscopic organism, in the nature of nematocysts from some form of coelenterate which is free.floating.”He also cautioned that seabather’s eruption should not be confused with “swimmer’s itch,” a dermatitis involving exposed areas of the body caused by Schistosome cercaride, a free swimming parasitic flatworm found in FRESH water.
The term “sea lice” apparently originated during the 1950s and was used by local U.S. residents in describing the condition. This popular term persisted, despite efforts by scientists to discourage use of such an inappropriate designation. Sea lice are actually small parasites that affect fish.
Beach goers sought their own remedies for the seasonal itchy rash. Folk remedies included the use of garlic, athletes foot spray, lemon, hydrogen peroxide, witch hazel, rubbing alcohol, spray starch, Epsom salts, and meat tenderizer. Unorthodox attempts to obtain relief included fingernail polish, undiluted bleach, ammonia, gasoline and turpentine. These are especially notable because they were used on extremely sensitive areas of people’s bodies. The prevailing term, “sea lice,” also encouraged the inappropriate use of head lice medication.
When marine biologists at the University of Miami analyzed water samples collected during the periods when complaints of bathers increased, large numbers of cnidarian larvae were noted. Cnidarians are a group of marine animals that contain stinging structures known as nematocysts, and include jellyfish, corals, sea anemones, hydroids, and Portuguese Man o’War. There are more than 9000 species of this group of marine animals; however, it appears that the larval form of Linuche unqui culata, also known as a “thimble jellyfish,” is responsible for the outbreaks in South Florida and the Caribbean. This probable causative organism was identified after cultures were successfully grown to maturity from plankton tows collected during 1992 outbreak periods.
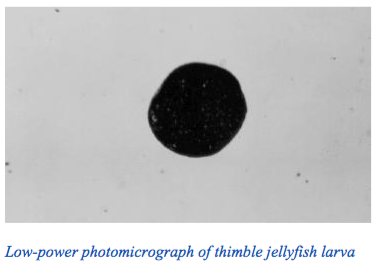
The suspected organism, barely visible except under excellent lighting, appears like a speck of finely ground pepper. Its size is approximately that of a pinhead floating on the surface layers of the water. The bathing suits worn by swimmers apparently trap variable numbers of larvae, with the fabric acting in a similar fashion to a net.
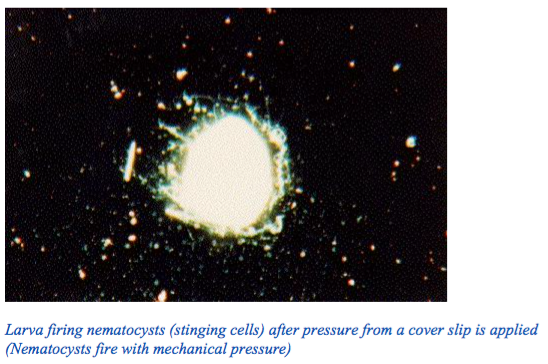
The many nematocysts surrounding each larva can be triggered to fire by mechanical pressure, such as in the friction areas of a bathing suit or bathing cap, or in body creases. A bather’s individual activities may also increase the amount of firing, such as contact with a surfboard, lying on the beach, or sitting on a car seat in the wet bathing suit during the trip home.
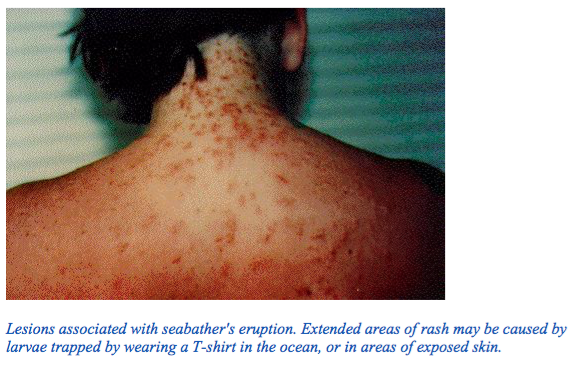
The surface area of a bathing suit may increase the area over which stings can occur. Female bathers wearing one-piece suits and children and adults wearing T-shirts in the water can increase the risk of a more severe reaction. It is not unusual to see evidence of 200 or more stings under a person’s bathing suit.
Changes in osmotic pressure may also activate the nematocysis. This could occur from evaporation as the bathing suit dries or from the bather’s rinsing with fresh water while wearing the suit. The nematocysts have been noted to have an affinity for hair as well as fiber, which could explain why people have lesions on their necks, from hair dangling in the ocean water and then contacting the skin.
The dermatitis usually becomes noticeable between 4 and 24 hours after exposure, although some persons do complain of a “prickling” sensation while still in the water. Persons who have had previous exposure to seabather’s eruption, such as lifeguards, tend to have immediate stinging sensations on re-exposure. Unfortunately, the only way that beach goers could be warned of the presence of this marine organism in the water was when lifeguards had the dermatitis during their early morning swims. Beach messages specifically warning about “sea lice” have been used since 1989 at access points to public beaches in Palm Beach County. However, no information is available for visitors entering many private beaches owned by hotels and motels.
Outbreaks of seabather’s eruption appear to be caused by shifts in South Florida’s currents, with the highest incidence of cases in such areas as Palm Beach County and Northern Broward County, where the Gulf Stream passes closest to shore. Other areas of coastline are affected by shifts in currents or by strong easterly winds bringing the larvae closer to shore. During initial outbreaks in early spring, adult jellyfish may be seen in the water. It is the larvae, however, not the adult organisms, that are responsible for seabather’s eruption. Once the adults die after spawning, the larvae continue to cause the outbreaks, with no mature jellyfish visible as a warning.
Lesions associated with seabather’s eruption have ranged from a barely discernible macular rash in those with no history of previous exposure to the largely typical maculopapular and occasionally vesicular eruption noted by most. Those with a history of exposure to the organisms have noted urticarial lesions at the onset of re-exposure. The dermatitis usually resolves within 1 week, although reactivation of initial lesions has been reported at intervals lasting several weeks or longer.
Probably because of the intense itching, many persons report difficulty in sleeping. Other symptoms include nausea, vomiting, diarrhea, headache, weakness, chills, muscle spasms, arthralgias, and a sense of malaise. It is unknown whether some of these symptoms reflect the ingestion of infected seawater or are manifestations of a systemic immune response. A retrospective case review of records of persons treated in an emergency department at the geographic center for seabathers eruption noted fever (temperatures
greater than 101 degrees F) in 8 of the 57 cases, All 8 cases occurred among children 11years of age or younger. The highest recorded temperature was 103.4 degrees F.
TREATMENT:
Treatment of this dermatitis currently includes the administration of an antihistamine, such diphenhydramine, for the itching and the application of an over-the-counter 0.5% hydrocortisone cream to the rash areas. Persons suffering from extended eruptions, with or without urticaria, or with recurrences of symptoms may benefit from the administration of epinepherine as well as oral or intramuscular steroids. A prescription for 1.0% corticosteroid cream can also be given.
Comfort measures include bathing in a colloidal oatmeal preparation and applying calamine lotion. The latter may be good for children, who benefit from its visual placebo effect. Diphenhydramine and calamine (Caladryl) lotion should not be applied when an oral antihistamine is being used to avoid toxic effects, especially in children. Caution is also in order, to make sure that steroid creams, in combination with oral steroids, are not overused. This may occur when large body surfaces are involved.
As noted, children with seabather’s eruption tend to exhibit febrile reactions more frequently than adults, probably because of their immune response. Parents should be observant and treat the symptoms. An additional recommendation for children is to clip their fingernails short, to avoid scratching of lesions.
Good personal hygiene, especially in the perineal area, will help patients of any age to avoid secondary bacterial infections. Should a secondary infection occur, as evidenced by purulent lesions that are not resolving, follow-up care with a dermatologist is recommended.
Any rash needs a thorough evaluation to rule out possible communicable causes. The key to the diagnosis of seabather’s eruption is a history of ocean exposure followed by the development of a dermatitis within 24 hours of exposure. Multiple persons within one household are typically affected. Persons with the rash of seabather’s eruption are not considered contagious.
PREVENTION:
Outbreaks of seabather’s eruption occur intermittently between March and August, but they appear to peak during early April through early July. There have been many days when no infestations have occurred. Beach goers need to listen to local beach reports and observe daily posted beach messages in affected areas. The following recommendations may also help in minimizing the number of stings:
1. Each beach goer needs to assess his or her individual risk of an immune response. Persons with a history of a severe reaction should confine their beach activities to land, or use pool facilities instead, during outbreaks.
- Swimmers should avoid wearing T-shirts while in the ocean. Use of a topical sunscreen and limiting sun exposure protects against solar injury. There is some evidence that use of a topical sunscreen or suntan lotion may actually protect skin from penetration by the nematocysts.
- Women should consider two-piece instead of one-piece bathing suits, to reduce the surface area of swimwear that could trap larvae. It is possible that smooth, tight weave bathing suits may trap fewer larvae than suits with an open-weave fabric.
- After ocean exposure, swimmers need to change out of their bathing suits as soon as possible after exiting from the water. Most lesions have occurred from contact with contaminated swimwear. Removal of possibly contaminated swimwear, followed by a shower to rinse off loose larvae, should limit the number of stings. If showers are in a public area, it is suggested that people bring a second suit to the beach; after removing the first, possibly contaminated suit, they can don the second suit and then shower. Showering with fresh water while still wearing a contaminated bathing suit could cause discharge of nematocysts trapped in the fabric of the suit.
- Bathing suits should be thoroughly washed with detergent and heat-dried after use. Some have experienced a recurrence of symptoms when wearing suits that had only been air-dried. Air-dried nematocysts still have the potential to fire. A person who has had a severe reaction may be wise to discard the infested suit.
Now that research of seabather’s eruption has begun, information to protect the public will be distributed as it becomes available.
REFERENCES:
- Sea lice survey. Boca Raton, Florida: Boca Raton Community Hospital. 1992.
- Lauther OC. The lonesome road. Miami: Center Printinq, 1963:91-2.
- Sams WM. Seabather’s eruption. Arch Dermatol 1949:60:227-37.
- Black NA, Szmant AM. Larval thimble jellyfish (Linuche unqui culata) as a possible cause of seabather’s eruption. Presented at 1992 Symposium on Flonda Keys Regional Ecosystem. Miami, Nov 18, 1992.
- Thorinqton GU, Hessinqer DA. Control of discharqe: factors affecting discharqe of crudes. In: Hessinqer DA. Lenhoff HM. eds. The biology of nematocysts. San Dieqo: Academic Press. 1955:232-53.
- Retrospective case review/medical records of SBE cases from 4/92-7/92. Boca Raton, Florida: Boca Raton Community Hospital, 1992.
- Heeger T, Moller H, Mrowietz U. Protection of human skin against jellyfish (Cyanea capillata) stinqs. Marine Biol 1992:113:669-78.